The RN is caring for client diagnosed with peptic ulcer disease . Vital signs done and reads blood pressure 88/42, pulse of 132, and respirations are 28. The nurse writes the nursing diagnosis “impaired tissue perfusion related to reduced blood volume.” What should the RN do First?
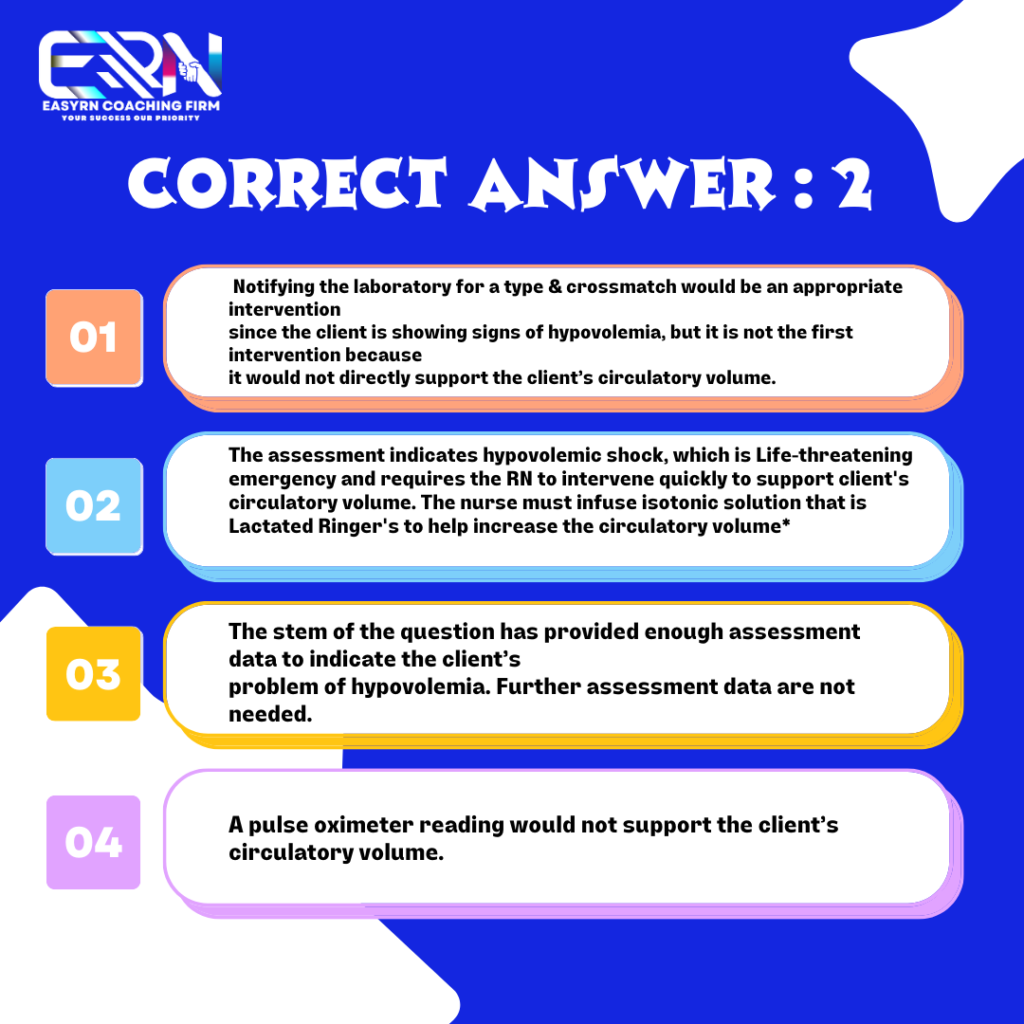
- Alert the laboratory to draw blood for grouping & crossmatch.
- Insert a 20-gauge catheter and infuse lactated Ringer’s.
- Assess the client’s abdomen for tenderness.
- Check the client’s pulse oximeter reading.
Post your answer in the comment section.
Author
-

Easy RN is the nation’s leading NCLEX coaching and processing firm. We’ve built our reputation on the ability to consistently produce a 100% NCLEX passing rate and match self-sponsored RNs (local and international) with healthcare institutions in the USA
View all posts


2
My answer is to first check the clients pulse oximetry reading becos of the impaired tissue perfusion related to the reduced blood volume
2
2
2
2
2
2
Since the impaired tissue perfusion is as a result of hypovolumia, the focus should be on increasing the blood volume
The best
2
2
2
3
2
2
Insert 20 guage catheter and infuse ringers lactate to prevent shock.
2, bcos patient is in shock with bp 88/42, patient is bleeding, for the first thing to do is to increase vascular volume, give iv fluid and RL (isotonic fluid).
2. Insert a 20-gauge catheter and infuse lactated Ringer’s.
The approach to answer this question is the use of the nursing process. The stem of the question have already provided you with the assessment data ie the vital signs and have given the nursing diagnosis.. you are to move to the next stage of the nursing process.. ie the implementation stage and in this stage your optimum goal is to improve tissue perfusion by increasing blood volume by inserting a 20 gauge catheter and infusing the lactated ringers
I agree with you
You are right
2
3
2
2
2
C
My answer is 2 but my question is why not cannula but Catheter
It’s the same my Boss
B
2
2
3
2
2
2
2
2
Give R/L ( an example of a volume expanded) to increase the blood volume to increase oxygen perfusion to the brain and to prevent hypovolumic shock.
2
2
2. Signs and symtoms of shock which the patient will need an isotonic solution to help meet the body demand
2
2
2
3
2
2
2
My answer is 2.